Wyszukaj w wideo
Arrhythmogenic cardiomyopathy. Pericardial diseases
I Międzynarodowy Kongres Kardiomiopatii – warsztaty z rezonansu magnetycznego serca
Podczas I Międzynarodowego Kongresu Kardiomiopatii eksperci omówili najważniejsze zagadnienia dotyczące tych schorzeń. Jakie trudności niesie ze sobą opieka nad pacjentem z kardiomiopatią?
Odcinek 4
Ostatni wykład w ramach warsztatów z rezonansu magnetycznego serca poprowadziła dr n. med. Anna Baritussio z Uniwersytetu Medycznego w Padwie, członkini zarządu European Association of Cardiovascular Imaging. Pierwsza część wystąpienia dotyczyła zastosowania rezonansu magnetycznego serca w diagnostyce i monitorowaniu chorób osierdzia, druga natomiast możliwości jego wykorzystania w arytmogennej kardiomiopatii.
Good afternoon. Thank you very much for the, um, invitation. Um, I'm going to talk about, um, pericardial diseases and how to use CMR and what to look for on CMR when it comes to assessing the pericardium.
Uh, just to begin with, we have to bear in mind that the pericardium is made of two layers. There's an outer, thicker layer that provides the structural support to the heart, and there's an inner, thinner, uh, layer that is closer, uh, to, uh, to the heart. Uh, normally, um, the pericardium has a thickness that is below two millimeters. And when it is abnormal and when it is thickened, it's usually greater than four millimeters in thickness. It has two sinuses and several recesses that we need to be aware of, uh, to, uh, avoid over-calling, uh, for a pathology. And it normally contains some fluid, so it's normal to see some traces of fluid, uh, because y- we can find up to 10 to 50 milliliters of, uh, fluid within the normal pericardium. And it has very important functions because we know that it limits cardiac motion within the chest, uh, and it prevents mainly infections and malignancies to spread, uh, from nearby structures.
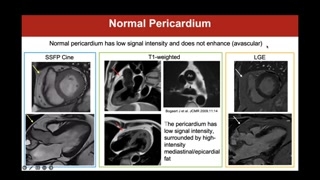
So how do we use CMR to look for the pericardium? Some people may tell you that we cannot see the pericardium in CMR. This is not entirely true, because, uh, normally the pericardium has low signal intensity in all CMR sequences, and we will see what I mean with all CMR sequences. And usually, when it's normal, it does not enhance because it is an avascular structure. We can see the pericardium on CINE sequences, you see these loops here, has a thin, um, structure with, uh, a low signal intensity. You see this black, uh, signal here as pointed by the yellow arrows. But usually, uh, when we want to see the pericardium, we need to bear in mind that it's usually surrounded by fat, and this is very useful for us to know because we can use dedicated sequences on CMR, especially the T1-weighted sequences that help us properly visualize, uh, fat as a very bright white, uh, signal. And these sequences, called T1-weighted sequences, are very useful to visualize the normal pericardium because, because we can, uh, see it as a low signal intensity structure within and surrounded by brighter fat. You see it, uh, here as, um, pointed at by the
red arrows, and you seehere, for example, a, um, asinus or a recess thatwe can see, uh, around, uh,the great vessels, which isabsolutely, uh, normal.And last but not least,we can still visualize normal pericardiumalso in late gadolinium enhancementsequences, and once again, it willappear, when it is normal,as a low signal intensity structurebecause the normal myocardium isavascular, therefore is not expected toenhance on post-contrast sequences, as,uh, pointed here by the whitearrows.
Of course, there are someconditions that are pathological, and Iwant to show you somebecause, you know, sometimes when wesee pathology once, then we'renot going to, uh, forget it,and we're going to recognizeit immediately.Uh, there is a conditionthat is called congenital pericardial absence,which can be, uh, completeor partial.Sometimes it is undetected untildeath, but other times it maybe very, m- dangerous, especiallyin the partial forms where the,um, uh, the, uh, partial,uh, pericardium may create, for example,some obstructions to the coronariesor, uh, to the heart itselffrom the outside.How do we recognize thata patient has congenital pericardial absence?There are some features thatare univocal.Once you see them, you'never forget them, and you willdefinitely recognize them again.One thing is that thecardiac apex will point posteriorly, andthis is specific of pericardialabsence because the r- pericardium, asI told you before, holdsthe heart in place, and inthis case, when we don'thave the pericardium, the heart shiftstowards, uh, the posterior.And the other thing isthat the absence of the pericardiumalso around the great vessels,uh, makes the, um, lung interposedbetween the aorta and thepulmonary artery.This is another marker ofcongenital absence.Another thing you may noteis that normally the heart doesn'tmove much within the chest,but when we don't have thepericardium that is holding, uh,the heart still, uh, in thechest, you, uh, can appreciatethat there's a greater motion ofthe heart with respect alsoto the lungs.But if we want tomake sure, we just said that,um, we can use theT1-weighted sequences because fat is verybright, and we need tosee a black structure s- usuallysurrounded by, um, by fat.And so if we applythe T1-weighted sequences in these patientswith congenital absence of pericardium,we may note, for example, thatthere is some pericardium aroundthe basal inferior wall or theleft ventricle here and surroundingjust part of the right ventricle,but you see that thereis no pericardium noted, noted inthe other, um, walls ofthe heart.So this is a caseof a partial, uh, congenital absence
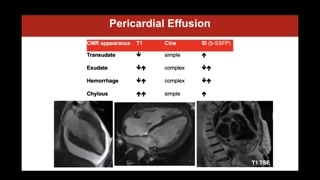
of the pericardium. But we mayalso look for pathology.For example, patients may bereferred, uh, to look for pericardialeffusion, uh, not for thepresence itself, 'cause that can, ofcourse, be, um, monitored anddiagnosed much easier and much easily,uh, with, with, uh, 2D,uh, transthoracic echocardiogram.But we may, uh, use,uh, the ability of CMR totissue characterize, uh, by usingthe different, uh, sequences to tryand understand the nature ofthe pericardial effusion.Because you see here, ifwe have a look of how,um, pericardial effusion may look,uh, on the cine images, onthe T1, weighted images,and on the postcontrast, you maysee that a simple pericardialeffusion, uh, has, of, of atrans- translated, uh, has avery simple appearance on cine, uh,images.As opposed to, for example,a hemorrhagic pericardial effusion, which usuallyhas a very, uh, complexappearance on cine sequences, but alsovery, very, um, uh, heterogeneous,uh, appearance on, uh, T1-weighted sequences.So, uh, it is veryuseful sometimes also to, uh, tryand characterize whether, um, whetherthe pericardial effusion that we're lookingat, uh, is simple or,for example, uh, as a high,um, protein, um, component.Therefore, uh, we may, uh,want to, uh, study patients withsuspected or, um, uh, confirmedpericarditis.
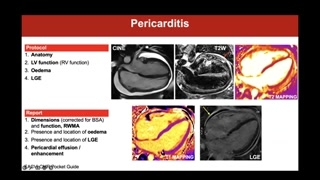
And if we want tothink at a protocol, we wantto look at, uh, tostudy a patient with suspected orconfirmed pericarditis, of course weneed to have the anatomy becausethat's very important, localizer sequencesto see, uh, where the heartis and to plan allthe sequences.We want to assess biventricularfunction, but we're mainly interested, uh,to look for edema onT2-weighted sequences that may be eitherstandard T2-weighted sequences or theparametric mapping with a T2 weighting.And then we want tolook at late gallium enhancement sequences,uh, to see for lategallium enhancement.And in this case, whatwe can see, there's, um, uh,thickened pericardium.You may probably more easilyappreciate it on the T2-weighted andthe postcontrast sequences.There's circumferential pericardial effusion.It has a very simple,um, appearance on the cine,images, although it is abit dishomogeneous or heterogeneous on theT2-weighted, so there may bea, a proteinaceous component.But what is interesting, uh,here is that the thickened pericardiumis diffusely edematous on theT2-weighted sequences.So there is diffuse pericardial
edema as shown by increased, um,signal intensity with this verybright white signal intensity here onthe T2-weighted, um, sequences, whichcorresponds to areas of marked lateenhancement.And you can, um, clearlyappreciate here that we have athickened pericardium of both layers,the outer and the inner, andyou can clearly see thatboth the inner and outer layersof the pericardium are markedlyenhanced.And we said this isabnormal because normally the normal pericardiumis avascular.We may also use parametricmapping nowadays, uh, to see howthe pericardium appears on theseparametric mapping sequences.And you can appreciate herenormal values should be, should havethis, uh, purplish, um, appearance.And you probably might appreciatehere that, uh, the pericardium isvery, uh, orangey, which meansthat there are increased T2 valuesand this is consistent onceagain with, uh, pericardial, um, edema.So we have a patientwith thickened pericardium, circumferential pericardial effusion,pericardial edema, and late enhancement,and this is consistent with acutepericarditis.
But we may also, uh,with CMR study the advanced stagesof pericarditis when it, uh,becomes a chronic process and wecan study patients with constrictivepericarditis.We have to look forbasically the same signs we willlook for on echo.We may look for theabnormal septal motion, like the septalbounce.We may look for abnormalregional wall motion abnormalities because theheart is fre- frequently, uh,tightened within the thickened pericardium.We have to look forpericardial thickness.You see here that thepericardium is thickened, uh, but youhave to bear in mindthat you may have constricted pericarditisalso with a normal pericardialthickness.So don't be misled bythis.So you need to lookat physiology and you n- needto look for the abnormal,uh, septal, uh, motion, uh, throughout,uh, breathing, uh, to lookfor, um, abnormal, uh, pericardial physiology.And then you may lookfor secondary findings, uh, that supportthe suspicion of constricted pericarditissuch as, for exam- uh, forexample, dilated atria as wehave in this case or adilated, uh, venous system likethe superior and inferior vena cavaor mainly, or also lookingfor secondary signs like the presenceof pericardial effusion or, uh,ascites.Unfortunately, we don't just see,uh, pericardial effusion or constriction whenit comes to pericardium, butwe may also, uh, uh, encounter
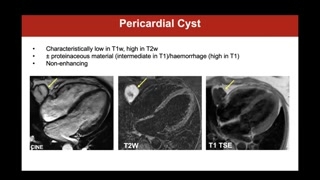
the presence of pericardial masses,uh, that may be benign butalso sometimes malignant.Uh, one of the mostcommon benign masses that we may,um, see when it comesto pericardial diseases is a pericardialcyst.Uh, CMR is very usefulas compared to, uh, mainly echo....Uh, because of the abilityto provide tissue characterization.And for example, pericardial cystusually have a very high signalon the T2 weighted sequencesbecause they're, they're, basically they havethe, uh, water component thatmake it appear very bright onT2 weighted sequences, and theyusually have a very low signalon T1 weighted, um, uh,sequences.Uh, of course it depends,the, the, the appearance of acyst on these sequences alsodepend on what they're made of,because if they have alot of proteinaceous material or theycontain hemorrhagic, um, product, uh,they may change their appearance.And for example, if wehave hemorrhage, as we've seen forpericardial effusion, we will findvery high heterogeneous signal, uh, onthe T1 weighted, um, sequences.Usually bear in mind thatcysts, uh, should not, uh, enhance.Sometimes they do enhance ontheir outer layers, on their, uh,on the capsule, but notreally enhance, uh, in the inside.
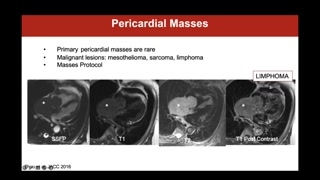
Um, mass, pericardial masses usually,uh, as a primary lesion, they'revery rare, but the pericardiummay host, um, uh, the, thepresence of secondarism to, uh,um, neoplasms that, uh, are originallylocated somewhere else.And we may find pericardiallocations in some specific, um, tumors,like for example, mesothelioma, uh,sarcomas, but very frequently, uh, lymphomas.And in these cases, itis very useful to have, touse a very, very broadprotocol that includes CINI sequences, theT1 and the T2 weightedto see, uh, how the tissuecharacterization of these masses is.We need to use restprofusion to understand whether the massis profused or not, becausethis helps understanding about the differentialdiagnosis.Uh, we may want to,um, use a parametric mapping or,um, the, um, T1 andT2 weighting with, with a fatsaturation to look for, uh,fat components, and then of course,the late-gallium enhancement sequences.So usually in these cases,we have to use a verywide, uh, protocol.And, um, this is because,for example, you see this caseof lymphoma where we seea very huge mass that invadestotally, um, the, uh, the,uh, the atrium and, uh, it
in- it, it infiltrates thepericardium as well and is verybright on the T2 weighted,is iso-intense to the myocardium onthe T1 weighted, and it,um, it's, uh, it gets, um,contrast, it's, um, really, um,heavily, um, vascularized on the post,uh, contrast, um, sequences.Uh, of course, uh, personally,I don't remember by heart allthese, uh, all the waythese details on how the masses,uh, behave on the differentsequences, but it's very useful toknow where to go andhave a look at, uh, whenyou need to understand abouta mass.And you basically have alook of how a mass behavesin a different way t-to try and get a, uh,differential, uh, diagnosis.
So, uh, to conclude, sowhat do, should you report aboutwhen you look at pericardialdiseases?Well, first of all, youneed to describe whether you seeany pericardial effusion and tryto characterize, um, if it's asimple or a proteinaceous ora hemorrhagic effusion.Of course, bear in mindto comment about pericardial thickness, especiallyif it is increased.Uh, then you have tocomment on the presence of pericardialedema and/or late gallium enhancement,and then comment on physiology.Is there a septal bound?Is there a dilated venoussystem?Is there evidence of pericar-uh, pleural effusion or ascites thatare not explained by other,um, features?And last but not least,if you're looking at a mass,try to have a verycomprehensive, um, protocol because of courseCMR will never provide histology,but you can be very preciseand provide the clinicians withsome differential diagnoses that may bethen very useful, uh, puttogether in the clinical context andhelp guide, uh, further management.Thank you for your attention.Uh, good afternoon, um, again.
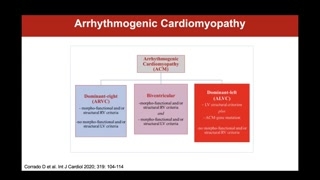
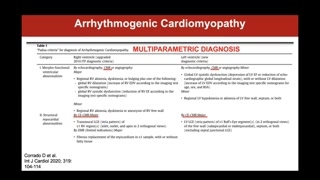
Thank you for the opportunityto, uh, talk also about, uh,arrhythmogenic cardiomyopathy.So, um, you may beaware of that, um, this diseasewas ori- originally thought, uh,to be a disease of theright heart, and it wascalled arrhythmogenic cardiomyopathy, um, of, ofthe right ventricle.Um, but it has beenshown, um, over the years thatthis disease may have eithera biventricular or a mainly leftventricular, uh, involvement.And it is now therefore,uh, called or known as arrhythmogeniccardiomyopathy that may have adominant right, a biventricular, or adominant, um, left, um, involvement.And, um, the, um, thediagnostic criteria, um......Uh, of arrhythmogenic right ventricularcardiomyopathy date back to, uh, 2010.Uh, those are the taskforce criteria.But more recently, in 2020,um, the, a, a group ofexperts has, uh, proposed a,a new, uh, sort of classificationthrough these, uh, so-called Padwellcriteria to, um, include, uh, these,um, other, uh, not reallyvariants, but these are the wayof, um, manifesting of adisease.And also, to include morewidely, um, specifically, to be honest,uh, CMR, uh, and itsability to provide tissue characterization, andby doing so, to, uh,detect some of the, uh, disease,uh, features.We have to bear inmind that arrhythmogenic cardiomyopathy is amultiparametric diagnosis that should neverrely on a single test.
So, even if you havea, um, suggestive, uh, CMR, youshould not, uh, definitely callthe disease unless there are otherparameters that fit in theclinical scenario.But if we have toconsider the role of CMR inthe diagnosis of arrhythmogenic cardiomyopathy,which is what I'm asked todo today, uh, we haveto m- w- to bear inmind that CMR has, uh,two, um, roles, let's say.One, uh, is about lookingat regional wall motion abnormalities ofboth, uh, ventricular chambers, um,because you know that, uh, thedisease is characterized by akinesia,dyskinesia, or bulging of both leftand right ventricular walls, andit should be, um, uh, ithas to be, uh, associatedwith either a dilatation of theheart or a dysfunction of
the heart, meaning by that leftor right ventricle, or both.But the second area, thesecond role of CMR, really comesfrom the ability to providetissue characterization, which is mainly basedon the, uh, assessment ofthe presence of late gadolinium enhancementthat usually has a knownischemic pattern, and it may involveat least one right ventricularregion to m- meet diagnosis, andat least one, uh, segmentof the left ventricle, uh, to,um, meet the criteria forthe left ventricular involvement.
Why CMR in arrhythmogenic cardiomyopathy?On one hand, CMR isa gold standard for the assessmentof biventricular volumes and function,so it is the gold standardalso to assess the rightventricle that is frequently not easilyseen and not easily explored,uh, on, on CMR, on echo,sorry.And on the other hand,uh, to provide tissue characterization andlook for the hallmarks, uh,of right ventricular or left ventricularor biventricular arrhythmogenic cardiomyopathy, whichis the fibro-fatty infiltration of theheart.And we will see whatI mean by that.
Uh, when we need toscan a patient with suspected orknown arrhythmogenic cardiomyopathy, we alwayshave our anatomy stack, because weneed to see where theheart is and to plan allthe sequences.We need to have oursequences to assess biventricular, uh, function,and we get to havesome specific, uh, approaches, hm, tolook for right ventricular regionalwall motion abnormalities, and I' showyou some examples.And then, we have thetissue characterization, which is, uh, mainlya T1-weighted pre-contrast, which isoptional, uh, to look for fatinfiltration, and the T1-weighted post-contrast,which is the late gadolinium enhancementto look for the sp-typical known ischemic, uh, LGE.
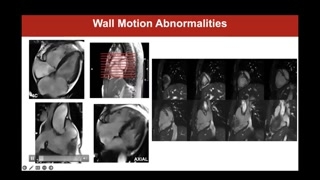
So, we said that, uh,CMR is useful when we getto, uh, l- look atpatients with arrhythmogenic cardiomyopathy, because itis the gold standard toassess biventricular volumes and function ina way that is totallyfree of any geometric assumption.And we get to clearly,uh, assess and provide the measurementsof biventricular volumes, of strokevolumes of both cavity, of ejectionfraction of both the leftand the right ventricle.But we said that weneed to look at regional wallmotion abnormalities, and if it'svery easy to look for regionalwall motion abnormalities of theleft ventricle, we're very used todo that on the short-axissequences.It may be not asusual or not as common tolook for regional wall motionof the l- uh, right ventricle.
And we can look atthe right ventricle, of course, onthe short axis, but wecan get specific sequences as, forexample, uh, the so-called threechamber, where we have, uh, wecan explore the inflow ofthe right ventricle, the apex andthe outflow, which, if youremember, is the so-called triangle ofdysplasia, so the three areasthat are mainly affected by, um,arrhythmogenic cardiomyopathy when there isa right ventricular involvement.And you see here, thereis a wide bulging of theRVOT, uh, just below thepulmonary valve.Of course, we can usealso the standard long-axis sequences, whereyou can appreciate here, forexample, in this four chamber, thatthere is an akinesia ofthe mid-cavity, uh, to apical, um,uh, three wall. But we mayalso have an axial stack, whichbasically, uh, cast the heartas we, we would with, um,with a cardiac CT orwith a CT of the thorax,and this allows us toexplore all the anterior, um, uh,portions of the right ventricle.And as you see here,we can explore the entire threewall of the left ventriclefrom just below the pulmonary valve,to the diaphragm, to see,for example here, that there isa, a regional wall motionabnormality of the three wall.Of course, we can alsohave some 2D, um, view ofthe left vent- the rightventricle, wh- where we, um, appreciatethe diaphragmatic and, uh, theanterior wall.And all of these needsto be looked at very carefullyto look for akinesia, dyskinesia,bulging.Bear in mind that hypokinesiais not among the criteria forarrhythmogenic cardiomyopathy.Needs to be proper regionalwall motion abnormality.
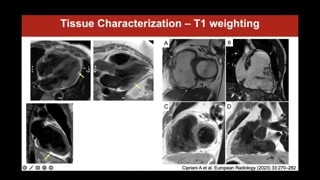
Uh, we said that wecan use, uh, CMR to tissuecharacterize and look for the,uh, features, uh, of arrhythmogenic cardiomyopathy.You know that this diseaseis characterized by fibro-fatty infiltration ofboth, uh, ventricles, and weare very lucky with CMR becausewe can, uh, look forfat infiltration of the myocardium, andwe do so by usingthe so-called T1-weighted sequences that arecharacterized a very bright fat,as you see here from thebright subcutaneous fat.And you see that thereis a bright fat here surrounding,uh, the heart as thisnormally happens.But what is interesting isthat we may get to seesome areas of fat infiltrationof the myocardium.Uh, please look here howthin the normal wall of theleft ventricle here is, andhow important this area of fatinfiltration, uh, is in the,um, mid-cavity to apical, uh, inferiorwall.And you get to seeother areas of infiltration, uh, here
as well in the, uh,basal to mid, um, posterior wallof the left ventricle.But likewise, you may want,you may happen to see fatinfiltration also of the rightventricle, usually when you appreciate alsoregional wall motion.Of course, it is moredifficult to see fat infiltration ofthe right ventricle because it'svery, very thin.But if you spot akinetic,dyskinetic areas of bulgings of theright ventricle, please carefully lookfor fat infiltration on the T1-weightedsequences.Of course, the diagnostic sensitivityand specificity, uh, of, um, these,uh, sequences, uh, uh, in,uh, right ventricular rather than leftventricular, uh, arrhythmogenic cardiomyopathy isslower, as we just said, becausethe, the right, not onlybecause the right ventricular wall isthinner, but just also because,uh, normally the right ventricle issurrounded by fat, and thismay create some confusion.And also bear in mindthat myocardial fat per se isneither a sign of diseasenor a sign of arrhythmogenic cardiomyopathy,so it needs to putinto context.But if you want toperform these sequences, this may beof help, um, uh, inthe, um, final diagnosis.
Uh, sometimes we will, wemay want to use, uh, othersequences to look for fatinfiltration.For example, nowadays, we frequentlyuse parametric mapping in our, uh,exams, and these may helpconfirm the presence of fat because,for example, uh, you clearlysee it here.These are the same pa-same patient.This is a standard T1-weightedsequence where you see the subepicardialstria of fat infiltration thatcorresponds to this area of fatinfiltration here in the, uh,mid-cavity to apical anterolateral wall.Uh, how am I surethat this is, uh, fat?Because on T1-weighted, fat hasa very low, uh, signal.It's very black, as yousee here from the subcutaneous fat,because it's a, it hasvery low, uh, native T1, uh,values.
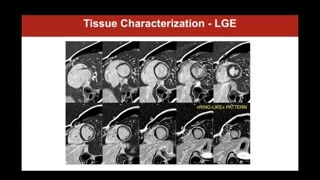
Last but not least, lategadolinium enhancement sequences are very usefulin arrhythmogenic cardiomyopathy.We need to look for,uh, non-ischemics, uh, l- late gadoliniumenhancement.Bear in mind that non-ischemicLGE usually spares the subendocardium andhas a subepicardial or mid-wall,um, distribution as in this casehere I'm showing you.And usually it does not,uh, follow, uh, the coronary distribution.So here you see wehave extensive non-ischemic LGE as aextensive epicardial, subepicardial stria ofthe, um, anterolateral wall from baseto apex of the anteriorwall here in the mid-cavity andin the apex and thebasal inferior wall, and here wesee that there is some,um, mid anteroseptal involvement as well.
And bear in mind, wealways have to compare the imageson two orthogonal planes, sowe check the long and theshort axes.And you see here inthese patients, you appreciate there's quiteextensive non-ischemic epicardial late enhancementof the lateral wall that theninvolves the anterior wall andthe septum as well in theso-called ring-like pattern that isvery typical and very specific ofthe left, um, dominant, um,arrhythmogenic cardiomyopathy, um, spectrum.Although in this case, youmay appreciate as well that wedon't get to see much,uh, the right ventricular wall andthis is because there islate enhancement here in the, um......In the, um, um, anterolateral,or let's say the free wall,um, in the mid-cavity andalso here in the, uh, diapha-fragmaticor inferior, uh, apical, uh,wall.And, um, it's very difficultsometimes to see, um, late enhancementof the right ventricle forthe same reasons why it's difficultto see fat infiltration becausethe right ventricle is very thin.But what I do tohelp myself is that usually we'ds- we should see, uh,the right ventricle on postcontrast sequenceas a black signal.And if I go around,I see the black signal ofthe wall here, but Idon't see anything here, and I'msure that there is wall,uh, at this level.So, uh, this helps mesay there is LGE of theright ventricle that, of course,it's usually transmural, uh, just becauseof the very, uh, lowthickness of the right ventricle.So bear in mind thatalthough it is more difficult, uh,we, uh, get to seeright ventricular late enhancement, and actuallythis is absolutely one ofthe features of the, uh, biventricularor right dominant arrhythmogenic cardiomyopathy.
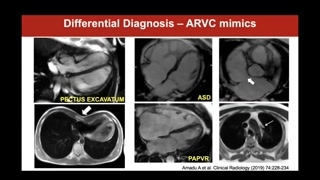
We have to bear inmind that, uh, especially if weuse other imaging modalities, specificallyecho, we may encounter some ofthe so-called ARVC mimics thatmay, uh, have us think thatthe patient has ARVC, andit is a different disease.And CMR in this caseis very useful.Bear in mind that itis usually very difficult to assessthe right ventricle of patientswith pex- pectus excavatum just becausethe heart, the right ventriclespecifically get, gets very odd shapeswhen there is pectus excavatum.So it's very useful tohave CMR so that you canreally appreciate very, uh, ina very detailed way, uh, the,uh, regional, regional wall motionand get proper assessment of, um,volumes and function.But also bear in mindthat the dilated RV, uh, usuallymake us think about arrhythmogeniccardiomyopathy, maybe especially young patients, butbear in mind that thereare different diseases.For example, this patient witha very dilated right ventricle hadan, uh, atrial septal defect,
and this, uh, case here onthe bottom, dilated right ventricle,dilated right atria.You see it's almost twotimes as big as the leftventricle.And this was a caseof a partial anomalous pulmonary venousreturn with the upper leftpulmonary vein draining into the brachiocephalictrunk rather than in the,uh, um, uh, left atrium, thereforedetermining a left to right,uh, shunting.So in conclusion, what shouldwe report when we look ata patient with suspected andall arrhythmogenic cardiomyopathy?
We have to report aboutvolumes and function.Bear in mind that nowadaysthe PADUA criteria recommend to usethe, um, references for normalvalues in the normal subject, andthis is because the previous,uh, 110 or one h- 100millimi- milliliters per squared meterthat were used in the taskforce criteria were based, uh,on the MESA cohort derived fromhealthy volunteers that were mainly,uh, 60 years of age, whereasHCM, ACM patients are usuallyvery young and often athletes, sothey get to have, uh,greater volumes just because of training.And also these reference valuesfrom the task force criteria werescanned with gradient echo CEswhile nowadays we usually use, um,um, SSFPCEs.And last but not least,you have to remember about tissuecharacterization and report about tissuecharacterization.
Although the T1-weighted sequences forfat infiltration are optional, please bearin mind that if thereis fat infiltration, you normally getto see it also onCini sequences, as it is inthis case, where you seethis very bright, uh, area surroundedby this darkish signal.And this is called Indiaink artifact, and it's very specificof fat infiltration.And last but not least,you should comment on the presence,the location, the extent, andmaybe the ringlike pattern of lategadolinium enhancement and look forthe fat infiltration and even moreso for late gadolinium enhancementof both ventricles.Thank you for your attention.
Rozdziały wideo
Pericardium anatomy and function
CMR techniques to visualize the pericardium
Congenital pericardial absence imaging features
Pericardial effusion characterization on CMR
Acute pericarditis: edema, mapping, and enhancement
Constrictive pericarditis, pericardial masses, and reporting
Arrhythmogenic cardiomyopathy overview and classification
CMR role and scanning protocol for arrhythmogenic cardiomyopathy
Right ventricular regional wall motion assessment
Myocardial fat infiltration and parametric mapping
Late gadolinium enhancement patterns and differential diagnosis